HMT
Description
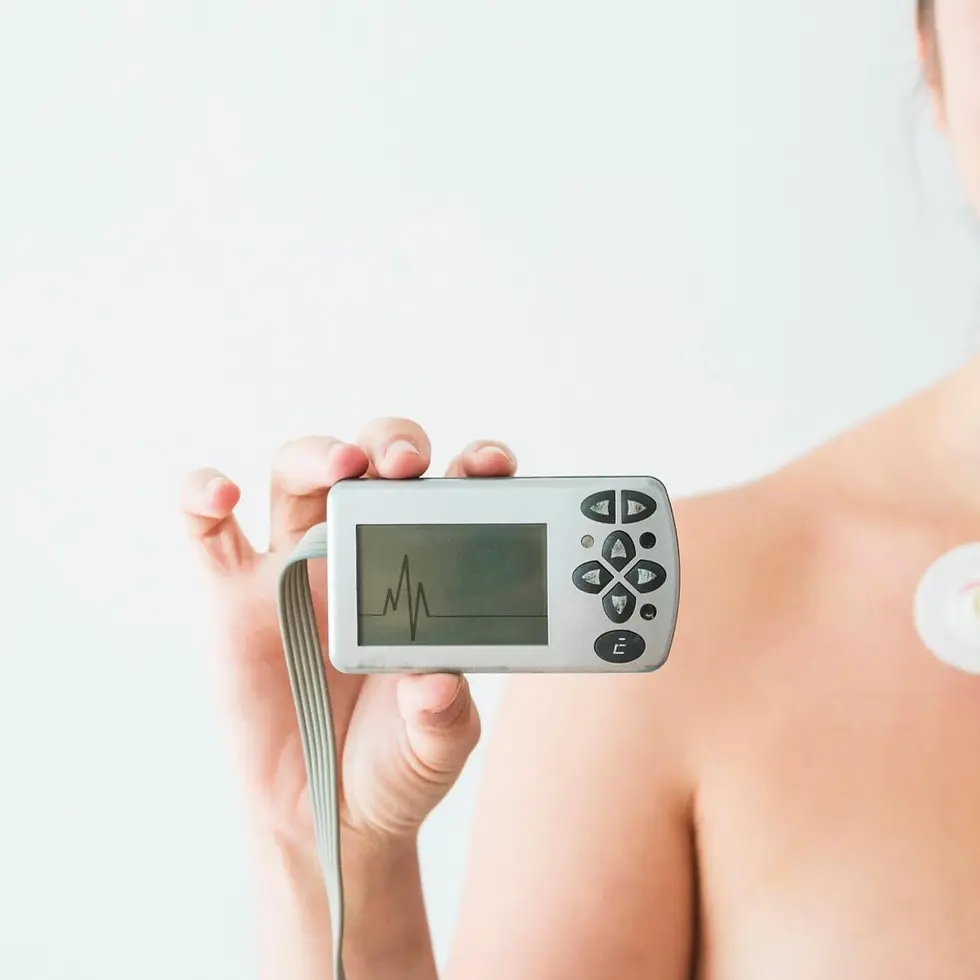
"Holter Monitor" test tracks your heart’s electrical activity continuously over 24 to 48 hours to detect irregular rhythms that may not appear during a standard ECG. Doctors may use this monitor when evaluating symptoms like fainting, skipped beats, or fatigue. Electrodes attached to a small device record your heart while you go about daily activities. Doctors analyze the results to identify arrhythmias or other cardiac concerns. Ongoing monitoring with a Holter supports accurate diagnosis and long-term heart rhythm management.
Category
Heart Function

Holter Monitor
Procedure
Non-Invasive
Sample Type
No biological sample is needed for this test.
Units
Not Applicable
Procedure Category
Measure
Test Group
Cardiac Assessment Group
Test Group Description
Cardiac Assessment Group: Tests within this group focus on evaluating various aspects of heart health and function. They provide insights into cardiac performance, identify potential risk factors for cardiovascular diseases, and assist in diagnosing conditions such as arrhythmias, coronary artery disease, and heart failure.
Key Reasons For Testing
Cardiac Rhythm Detection: Continuously monitors heart rhythm over 24–48 hours to identify arrhythmias like atrial fibrillation or bradycardia.
Symptom Diagnosis: Correlates symptoms like dizziness or chest pain with rhythm changes.
Treatment Monitoring: Assesses the effectiveness of antiarrhythmic medications or devices like pacemakers.
Syncope Evaluation: Investigates fainting episodes linked to arrhythmias.
Ischemia Detection: Detects transient ischemia during daily activities.
Comprehensive Monitoring: Offers detailed insights for sporadic arrhythmias beyond standard ECGs.
Results That Differ From The Norm (Direct and Indirect Causes)
Abnormal results may indicate:
Atrial fibrillation (Irregular and often rapid heart rate)
Bradycardia (Slow heart rate)
Heart block (Impaired electrical conduction within the heart)
Premature ventricular contractions (Extra heartbeats originating in the ventricles)
Tachycardia (Fast heart rate)
Ventricular fibrillation (Rapid, irregular, and chaotic heart rhythm)
Currently, this test is not directly associated with any conditions listed on the Health Status page. However, it may be included as part of a broader set of tests linked to specific health conditions.
Health Status Conditions It May Be Used To Assess
Some Prominent Medical Labs That May Offer This Test
Please note that this particular test has not been associated with any of the listed prominent medical labs. We recommend enquiring with your private physician or nearest hospital to determine where this specific test can be performed.
References
Important Note
Any medical procedure yielding results outside the norm may be directly or indirectly linked to the conditions outlined on this page. Various factors, including genetics, medication and supplement usage, recent illnesses, pregnancy, pre-test eating, smoking, and stress, can impact the test's outcome. Additionally, factors like false positives, false negatives, inaccurate analyses, and others can influence results.
Reference ranges, which help healthcare professionals interpret medical tests, may vary depending on age, gender, and other factors. They may also differ between laboratories due to variations in instruments and methods used. Optimal ranges are designed for preventive purposes, aiming to identify trends and potential risks early, while normal ranges reflect conventional laboratory values indicating no current disease or pathology. Your healthcare practitioner may have specific reasons for testing that deviate from the usual or may interpret results differently based on individual circumstances. Proper interpretation typically involves considering clinical findings and other diagnostic tests. Hence, it is crucial to provide your healthcare professionals with a comprehensive medical history, consult with them for result interpretation, and follow their guidance for potential re-testing or additional diagnostics.
Disclaimer
This content is provided solely for informative and educational purposes. It is not intended as a substitute for medical advice or treatment from a personal physician. Regarding the interpretation of their medical test results and/or specific health questions, it is recommended that all readers and viewers consult their physicians or other qualified health professionals. The publisher is not responsible for any adverse health effects that may result from reading or following the information in this educational content. Before beginning any nutrition, supplement, or lifestyle program, all viewers, especially those taking prescription or over-the-counter medications, should consult their physician or health care practitioner.
Please note that while prominent lab names are included in this content, we cannot guarantee that these labs offer all the tests mentioned. For confirmation, individuals should contact the labs directly or consult their medical practitioners. The information provided reflects general knowledge at the time of publication and may not include recent updates or emerging research. Readers should verify details with qualified professionals to ensure the most up-to-date and accurate guidance.
[1] Rensma PL, de Bruin AM, Coumel P, Hauer RN. Evaluation of the Holter monitor technique for ambulatory arrhythmia detection. J Electrocardiol. 1988;21(Suppl):S34-S40.
[2] Saxon LA, Uretz EF, Aberle LG, et al. Cardiovascular risk stratification by ambulatory ECG monitoring in community-dwelling older adults. Ann Noninvasive Electrocardiol. 1998;3(3):251-258.
[3] Carretero OA, Oparil S. Essential hypertension. Part I: definition and etiology. Circulation. 2000;101(3):329-335.
[4] Zareba W, Lin DA. Anticipating sudden cardiac death: predisposing conditions and risk stratification. J Cardiovasc Electrophysiol. 2003;14(8 Suppl):S102-S107.
[5] Theres H, Wieneke H, Neuzner J. Advanced ECG analysis techniques in Holter monitoring: Diagnostic accuracy of automated systems. Pacing Clin Electrophysiol. 1999;22(4):589-596.
[6] Lown B, Verrier RL. Neural activity and ventricular fibrillation. N Engl J Med. 1976;294(21):1165-1170.
[7] Gillis AM, Skanes AC. The use of ambulatory electrocardiographic monitoring. Can J Cardiol. 2000;16(6):725-732.
[8] Kennedy HL. Ambulatory (Holter) electrocardiography: past, present, and future. J Am Coll Cardiol. 1997;29(1):158-159.
[9] Goldenberg I, Moss AJ, McNitt S, et al. Time dependence of arrhythmic risk and implications for secondary prevention in patients with myocardial infarction. J Am Coll Cardiol. 2006;47(7):1301-1307.
[10] Buxton AE, Josephson ME. The role of Holter monitoring in patients with frequent premature ventricular complexes. J Am Coll Cardiol. 1992;20(4):929-933.
[11] Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. Circulation. 2008;117(21):e350-e408.
[12] Janse MJ, Lammers WJ, Kléber AG, Durrer D. Electrophysiological basis of ventricular arrhythmias detected by Holter monitoring. Circulation. 1984;69(5):912-918.
[13] Chiladakis JA, Kalogeropoulos AS, Arvanitis MS, et al. Ambulatory electrocardiographic (Holter) monitoring in detecting ischemia in patients with chest pain. Int J Cardiol. 1995;49(3):261-268.
[14] Kalra PR, Sharma R, Shamim W, et al. Clinical application of Holter monitoring in the management of heart failure. Eur J Heart Fail. 2001;3(5):565-569.
[15] Jenkins JM, Flaker GC, Price P, et al. Comparative efficacy of Holter monitoring and event recording in detecting asymptomatic arrhythmias in high-risk patients. Am J Cardiol. 1989;63(7):453-456.
[16] Peterson PN, Greenlee RT, Go AS, et al. Validation of arrhythmia detection in ambulatory ECG monitoring. Am Heart J. 2010;159(4):605-611.